Pediatricians say climate conversations should be part of any doctor’s visit
From low birth weight to wildfire smoke, kids can bear the brunt of climate change.

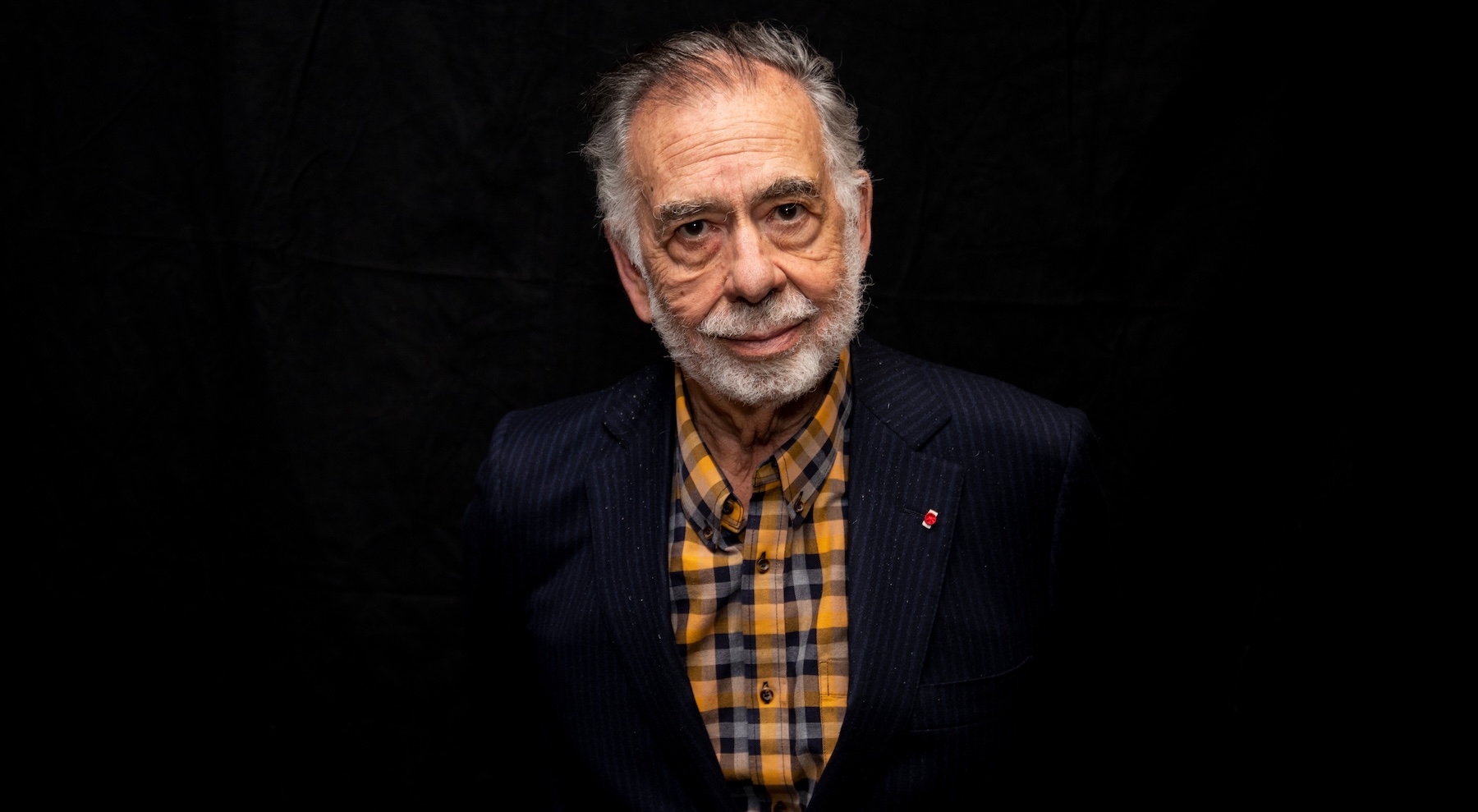
The reality of climate change came home for Dr. Samantha Ahdoot one summer day in 2011 when her son was 9 years old.
An assistant professor at the University of Virginia School of Medicine, Ahdoot and her family were living in Alexandria, when there was a heat wave. Morning temperatures hovered in the high 80s, and her son had to walk up a steep hill to get to his day camp.
About an hour after he left for camp, she received a call from a nearby emergency room. Her son had collapsed from the heat and needed IV fluids to recover.
“It was after that event that I realized that I had to do something,” she said. “That, as a pediatrician and a mother, this was something that I had to learn about and get involved in.”
Dr. Ahdoot made good on that vow. She is the lead author of the American Academy of Pediatrics’ newly updated policy statement on climate change, which appeared earlier this year. The statement urges pediatricians to talk about climate change to their patients. But research suggests that’s not happening very much yet, and there are practical barriers in the way.
Back in 2007, the AAP was the first national physicians’ group to make a public statement about climate change. The updated statement covers the growing research on the many ways climate disproportionately affects children in particular. Heat raises the risk of preterm birth; infants are among the most likely to die in heat waves. Because their bodies cool themselves less efficiently than adults, children remain more susceptible to heat-related illness as they grow. Children breathe more air per pound of body weight, making them up to 10 times more affected by toxins in wildfire smoke. Excess heat hurts children’s performance in school, especially low-income children with less access to air conditioning. And research suggests that teens and youth are feeling more climate anxiety than older adults.
The new policy statement’s number one recommendation is that its members “incorporate climate change counseling into clinical practice.” This may seem like a tall order, considering the average pediatrician visit is 15 minutes. A 2021 study found that 80 percent of parents agreed that the impact of global warming on their child’s health should be discussed during their routine visits. But, only 4 percent said that it had actually happened in the past year.
“How do you talk about climate change in a visit where you have to talk about X, Y, Z, do all the vaccines, answer every concern?” said Dr. Charles Moon, chief resident at the Children’s Hospital at Montefiore in New York. A member of the AAP Council on Environmental Health and Climate Change, he has been working to build a curriculum at his hospital to start teaching pediatricians and other doctors about this.
“I don’t think we have all the answers to that yet,” he said. “I do a lot of work teaching other pediatricians, and it requires a little bit of a mindset shift.”
Dr. Moon sees patients in the South Bronx, nicknamed “Asthma Alley” for its air pollution. Part of his challenge is putting environmental threats in perspective for families who face many different obstacles in their lives, in a way that doesn’t lead to despair or disempowerment.
Or, as he put it: “If you can’t put food on the table, who wants to hear about climate change?”
In Oakland, California, Dr. Cierra Gromoff has a lot of experience with families on Medicaid, and she says the pressure on them and their healthcare providers is real. “There are these already incredibly marginalized groups of kids facing other insurmountable things,” she said. “These providers have so little time, they have to focus on the biggest burning fire — whatever systemic problem is going on.”
A clinical child psychologist, Gromoff has been concerned about the environment since her childhood as an Alaskan Native in the remote Aleutian Islands. She thinks that to overcome these obstacles, state and federal insurance providers should require or reward doctors for taking the time to include environmental health in their assessments.
She is the co-founder of a telehealth startup, Kismet Health, which is building a tool that could show local environmental threats that are indexed to a patient’s home or school address.
The tool could help doctors recognize climate risks, by showing if a patient lives near a green space, an urban heat island, or a polluting chemical plant.
Gromoff said she would like to see free resources that pediatricians can give families on everything from the signs of heatstroke in a baby to eco-anxiety.
“We should have a screening question,” she said. “‘Are you worried about what’s happening to our earth?’ And if they say yes, we should be able to provide some type of handout: What you’re feeling is real. These are small steps you can take.”
The good news, say Moon and Ahdoot, is that interest in the topic is picking up in the medical community. Over half of medical schools are covering climate change in the curriculum, a number that’s more than doubled since 2019. And there are state research consortiums on climate and health in 24 states, Ahdoot said. The American Academy of Pediatrics has been creating continuing education materials on the topic as well.
Incorporating climate change into clinical practice is not about adding another item to an already long checklist, Ahdoot said. It’s also not about transforming pediatricians into activists, or talking about factors that families can’t do anything about.
“Pediatricians never want to be proselytizing,” she added. “It always has to be valuable to the individual patient.”
The goal of the new climate policy for pediatricians is to help doctors translate their climate knowledge into solutions and helpful advice for their patients. A few examples from Ahdoot include: running a test for Lyme disease for patients in Maine, which used to be too cold for ticks; beginning allergy medication in February because pollen arrives earlier in the year; or teaching athletes the warning signs for heat exhaustion.
For Ahdoot, it’s also important to be aware of how climate affects a child’s mental health. Part of the answer, she said, is talking about actions that families can take that benefit both people’s health and the planet, like eating more plant-based diets, and walking or biking instead of driving.
“What’s good for climate,” she said, “is generally good for kids.”
This story has been updated.
This story was originally published by Grist with the headline Pediatricians say climate conversations should be part of any doctor’s visit on Apr 19, 2024.
What's Your Reaction?